RAJ LAKHANPAL, MD, FACEP
CEO, SPECTRAMEDIX
Our personal information accumulates in nanoseconds. Data is gathered by banks, credit cards, smart devices, healthcare systems. Taken together it’s big data. From where we stop for our morning coffee, to whether we follow our PCP’s directives. Big data can be individualized to determine discrete behavior or analyzed to get the big picture. In hospital analytics, to optimize health outcomes while remaining financially viable requires the ability to see the big picture while caring for the individual.
As more data is amassed and stored it’s simplistic to think it automatically provides better insight. Data needs a common thread to make it useful, and that thread is not the patient, it’s the patient records. How can we improve data flow and clarity for referring clinicians; to provider networks as new beneficiaries enter and exit; and to the patients themselves, when multiple systems are in play and paper records still hold many secrets?
While HealthIT.gov reported in 2014 that one in three patients brought their medical history or test results when referred between clinicians, it also reported that 50% of physicians and 80% of hospitals had made the transition to electronic records a year earlier. So why are patients still carrying their records from Doctor A to Doctor B?
There are numerous players in the EHR (Electronic Health Records) arena. And that is a large part of the challenge. Competitors generally are not interested in sharing with each other. Yet, health records need mobility and communications capability. Data needs to travel with patients. Mergers of hospitals and large groups can result in the acquisition of legacy EHR software. Without resources to transfer all data to a single EHR vendor or a single software version, interoperability — even within health systems — can be difficult.
In 2010 as part of the federal HITECH Act, the Office of the National Coordinator (ONC) for Health Information Technology provided funding to states to help establish Health Information Exchanges (HIEs). HIEs securely share patient information between physicians, hospitals and the patient, but needs the right technology to normalize the data. Normalization, which creates the common thread among disparate data sources and records, is the key to interoperability. Normalization is what makes data useful on the population level. Normalization allows the high-level insight into a community or an attributed patient base to drive meaningful health and performance outcomes.
Merging HIE information with claims or billing data provides another level of evidence to promote cost savings and reimbursement opportunity. Are patients filling prescriptions? Are they keeping appointments with referred specialists? Have they visited an ED and could that visit have been avoided?
In a fee-for-service world, interoperability is less of an issue. Right now, we’re straddling the transition to value-based reimbursement. Data interoperability is critical to risk profiling, population health insight, cost management, work flow and staffing. When the transition to value-based payment is complete, which healthcare entities will remain viable will depend on their ability to maximize interoperability.
Aggregating claims and HIEs relies on technology that can normalize data, and then provide near real-time evidence that includes a unique identifier for each patient. According to the 2010 US Census, Smith is the most common surname in the US, so you will want to know if you’re looking at Mary A. Smith’s records or MaryAnn Smith’s records.
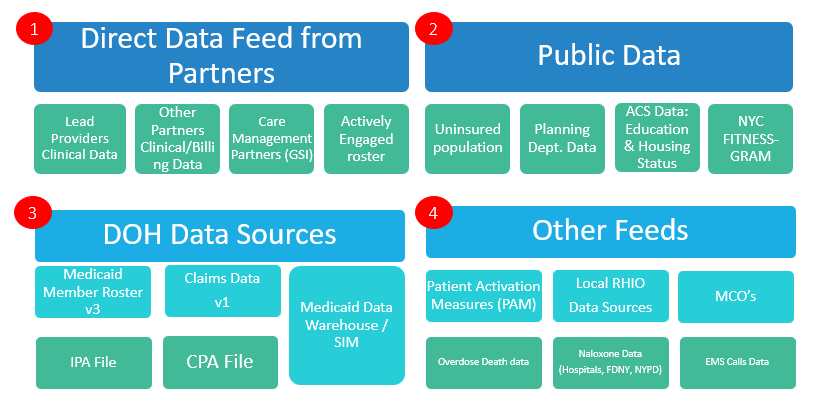
As a provider of value-based healthcare population analytics, SpectraMedix helps clients identify patients. We help hospitals and other entities to develop custom queries that use data from all available sources, including discharge notes (unstructured data) and living conditions (social determinants of health). The chart below shows just how many types of data are aggregated, in addition to HIE and claims, for one SpectraMedix Medicaid reform client.
Data analysis is leveraged in increasingly innovative ways. It can identify hot-spots – areas with higher-than-average substance use, for example. Working with community-based organizations can bring rehabilitation programs closer to those who need it. Analysis can locate neighborhood food deserts that may contribute to nutrition-related conditions such as diabetes. When operating within a value-based payment model, clinicians and health systems may find that “treating” the lack of fresh, affordable food is financially more rewarding and sustainable than treating individuals’ escalating chronic conditions.
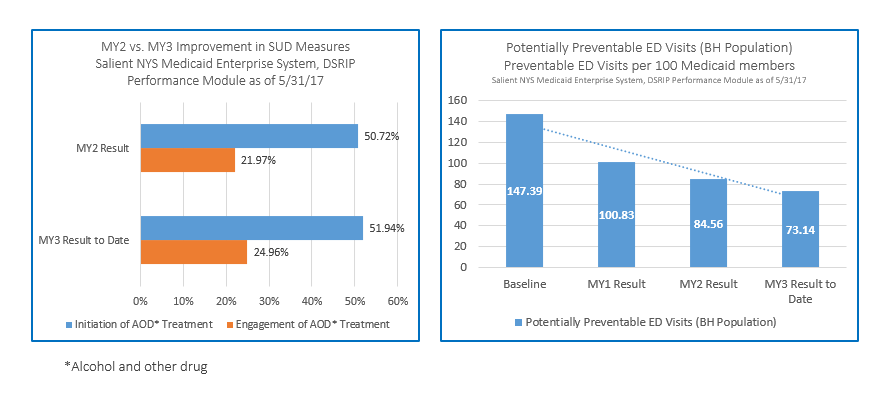
Within the scope of Medicare, interoperability and cost are two of four drivers for reimbursement. CMS uses billing as the primary data source for cost. Preventable hospital admission or readmission will show up in billing data, but the lag between a procedure being billed and a clinician seeing that data can mean an avoidable ED visit has already occurred or that tests have been duplicated. Integrating data from an HIE identifies issues that affect patient outcome and financial performance. Interoperability stimulates coordinated care.
Bringing care closer to the patient, encouraging lifestyle changes through education, and contacting patients who miss appointments or fail tests (chase lists) improve patient health and clinicians’ bottom line. Change within healthcare is more than new medications or procedures. It increasingly is about the issues some individuals face at home, whether that’s stress, poor diet or no home at all. Treat the patient and the disease. Analytics makes it possible.
By the way, remember that donut you grabbed with your morning coffee? It may become part of your health record in ways you never imagined.
Dr. Lakhanpal presented on HIEs, Billing and Population Health at the 2018 NJ HFMA 42 Annual Institute

