VBP Strategy: Nine Value-Based Payment Predictions for 2024
*Contributions to this blog post were provided by Rahul Lakhanpal, Chief of Staff at SpectraMedix, and Sean Kelly, Senior VP, Growth and Business...
.png)

The number of value-based contracts across the healthcare industry is rapidly increasing, yet many health plans still struggle with the value-based contracting process. A primary reason for this is that payers do not have the resources or expertise to manage all of the different components that go into creating and implementing contracts that improve quality while yielding savings. Additionally, health plans must convince skeptical providers that value-based contracts are designed to be mutually beneficial arrangements.
An effective value-based contracting process needs to allow health plans to design and evaluate performance scoring methodologies, risk assumption options, and other contract terms across all lines of business. It should empower them to collaborate with their provider networks to identify, evaluate, prioritize, and impact the value levers or performance indicators that affect utilization, cost, and quality.
In this blog, we’ll present key questions that payers need to answer as they continue to navigate the disruptive process of adopting value-based contracts, and lay the foundation for creating mutually beneficial arrangements that lower costs, improve quality, and produce better outcomes.
It’s incumbent on health plans to determine how best to prioritize these challenges based on the make-up of the organization and the needs and goals of the organization. Addressing these challenges involves significant, often overlapping, effort from the various stakeholders. Utilizing analytics to recognize and assess starts the journey, while operationalizing the mechanics of reimbursement finishes it. In the end, better patient outcomes at lower costs is the overarching goal.
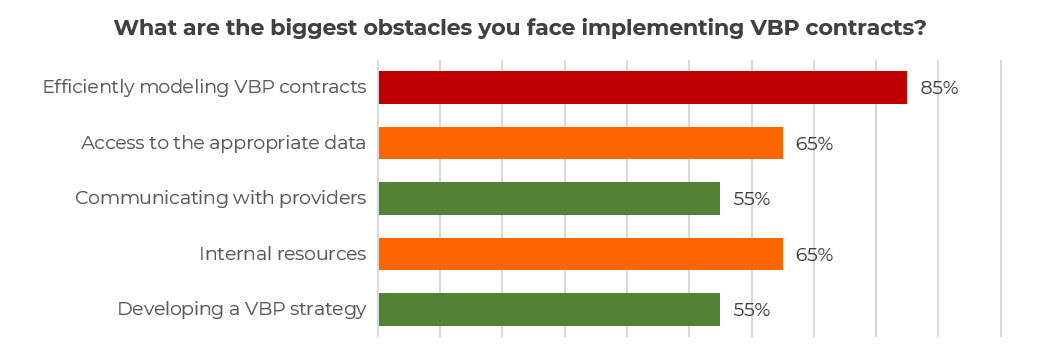
Last year, SpectraMedix conducted a poll of health plan executives and professionals, asking “What are the biggest obstacles you face in implementing VBC contracts?”
VBC contracts are often developed as one-offs, using excel or some other similar tool. Health plans require a system that allows team members who are not sophisticated with VBC contracting to model and create a contract without specialized knowledge. Plans need to be able to do this before negotiations even begin so that they can decide what types of contracts and terms to offer their provider community. If plans are in direct negotiations, they need to be able to run a pro forma analysis that follows the terms of the proposed contract using the plan’s own data to understand how that contract would work and the providers’ baseline performance moving forward. The tools and process should support commercial, Medicare, Medicare Advantage, and Medicaid business lines across the entire spectrum of VBC types, including shared risk and full capitation.
Why do health plans need to have the tools and processes in place now to develop and scale value-based contracts?
Health plan executives have a difficult task in implementing more risk-based contracts with their providers. Ultimately though, it is to everyone’s benefit—payer, provider, and patient—as the long-term objective is to improve quality and lower costs. A payer’s ability to identify and prioritize the value levers that have the biggest impact on performance, and then pull those value levers to improve performance, will come out ahead. To achieve this, payers need a solution that is:
.png?height=150&name=SpectraMedix%20-%20Stacked%20Logo%20(1).png)

*Contributions to this blog post were provided by Rahul Lakhanpal, Chief of Staff at SpectraMedix, and Sean Kelly, Senior VP, Growth and Business...

A risk bearing entity, whether it is a health plan, an ACO, or an IPA, should consider including SDoH contracting into their Value-Based Care (VBC)...