How Linking Clinical Gaps to Reconciliation Drives ROI
Welcome to Part Two of our series delving into the critical aspects of financial reconciliation in value-based care (VBC) contracts for risk-bearing...


Timely and accurate financial reconciliation is a critical part of any value-based contracting process. Effective contract reconciliation in all lines of business (MSSP, Medicare Advantage, Medicaid, Commercial contracts) and for any type of contract (shared savings, shared risk, capitation, Medical Loss Ratio, total cost of care) needs to align contract terms, data availability and integrity, medical and drug costs, quality measure results, and other key value levers across the full life cycle of the arrangement. The ability to do this can be the difference between positioning your organization for success or failure in VBP arrangements.
In this blog post, I will identify four essential components of financial reconciliation that all risk-bearing entities should adopt as part of their value-based contracting process.
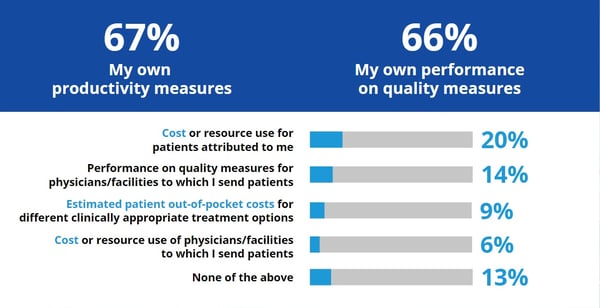
Most providers believe value-based contracting will expand over the next several years. However, the critical missing piece is that two-thirds of physicians have access to their own productivity and quality performance data, but very few have access to cost information, a key component of the financial reconciliation process.
SURVEY: What types of performance information are available to you and other clinicians in your organization?
The Importance of Timely and Accurate Financial Reconciliation
The two key factors to ensure successful contract reconciliation are timeliness and accuracy. Frequent reconciliation is important because for most value-based contracts, shared savings/losses are due at the end of the year. End-of-the-year financial reconciliation implies no feedback was available throughout the year to drive performance improvement that can lead to positive financial outcomes.
The key steps in undertaking VBC financial reconciliation are as follows:
1) Understanding Your Contract Portfolio:
As value-based contracting expands, it will become more complex and risk-based. Risk bearing entities (Health systems, ACOs, and providers) need to understand different risk-sharing methodologies that can be used to craft a value-based contract, including:
Within each of these methodologies, every contract is different. For example, different shared saving contracts could have different quality adjustments, risk-sharing corridors.
Additionally, contracting teams must understand and navigate key contractual elements, including covered services, carve outs, performance period, risk adjustment, bonus payments for meeting quality benchmarks, patient attribution, provider network-employed or affiliated, payment terms, and so on and so forth. With these elements in place, you can get a baseline to understand common denominators and key differentiators across the portfolio.
2) Implementing a Data Strategy:
Risk bearing entities need a holistic data strategy to accommodate value-based risk methodologies not only for financial reconciliation, but also to run performance analytics and contract scenarios. Each payer’s data is in its own format spread across disparate systems and stewards, so receiving it poses a variety of challenges that need to be overcome.
It's critical to create an inventory of your data to understand its availability and shortfalls and plan accordingly. In addition to this, contracts must clearly define and establish data reporting and submission responsibilities. This is a topic for another blog that I will be writing shortly.
3) Setting up Reconciliation Requirements:
There are several decisions to be made while setting up the process of monthly reconciliation:
4) Financial Reconciliation Leading to Performance Improvement:
The key indicators that risk-bearing entities should consider as they evaluate performance and take actions to improve contract results are as follows:
Conclusion:
These key insights will greatly enhance your ability to take on risk in your value-based contracts. In a follow-up blog, I will expand on step two and explore advancing from financial reconciliation to performance improvement.
In the meantime, I welcome your thoughts on this topic. Please feel free to email me at raj.lakhanpal@spectramedix.com with any questions or comments you’d like to share.
References:

Raj Lakhanpal

Welcome to Part Two of our series delving into the critical aspects of financial reconciliation in value-based care (VBC) contracts for risk-bearing...

Risk-bearing entities such as hospital systems, IDNs, and IPAs are central actors in the stage play that is the value-based care (VBC) revolution....