Value-Based
Contract Modeling
Design, Evaluate, and Simulate Successful Contracts
Designing value-based contracts is a complex and time-intensive process that relies on fragmented data and intricate spreadsheets for contract modeling and evaluation.
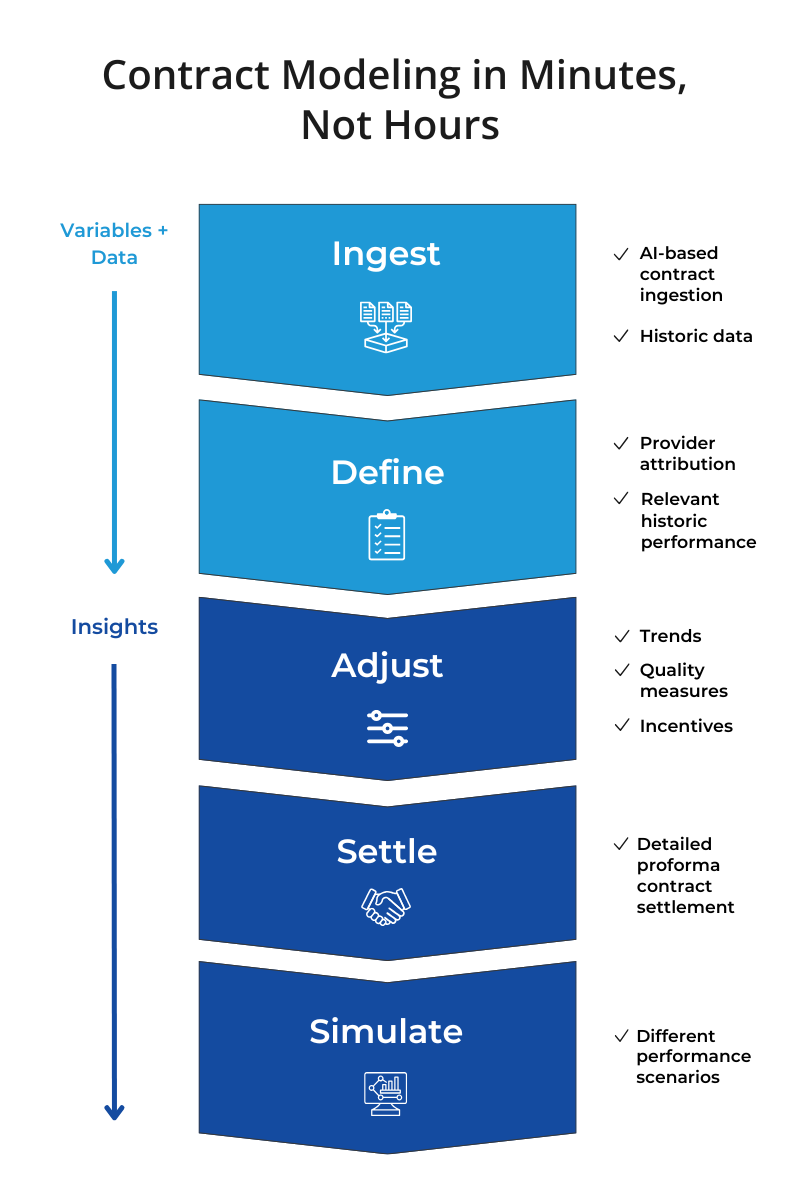
The AI-enabled SpectraMedix Contract Modeler streamlines this process, drastically reducing the time required to design and simulate value-based contract performance. This purpose-built solution for value-based contract development empowers health plans and health systems to evaluate the financial impact of different contract types, provider networks, and performance scenarios across all lines of business.


Smarter Contract Modeling to Empower Negotiations
Simulate financial performance across multiple parameters, performance levels, and risk-sharing arrangements to improve negotiations and align with organizational objectives.


Simulate Financial Impact—Model the effects of quality, utilization and risk scenarios across various contract types and payout structures.

Predict Provider Performance—Evaluate top and underperforming providers to optimize network alignment and incentives.

Standardize Contracts—Streamline contract creation and negotiations with reusable, pre-designed templates.

Leverage Historical Data—Build contract models rooted in your providers’ unique data, ensuring trends and insights reflect your market.
.jpg)
Where Do You Fit In?
The SpectraMedix VBP platform empowers users across your health plan's value-based care enterprise with solutions to your specific, role-based challenges and pain points.

Ready to Delve Deeper?
SpectraMedix is here to help you crawl, walk, or run toward your value-based payment goals. Contact us today to find out how we can help you more effectively manage and expand your value-based portfolio across all lines of business.








.png?width=75&height=75&name=analytics-team%20(2).png)